By Jonathan Korostoff, D.M.D., Ph.D.
Upon initial presentation, the patient was a normally developed 23-year-old Caucasian male with a history of ectodermal dysplasia. He had undergone orthodontic treatment as an adolescent and his desire was to replace his missing teeth with implant-supported fixed restorations.

Upon review of his medical history and extraoral examination (Figure 1) it was evident that the sole manifestation of his ectodermal dysplasia was agenesis of numerous teeth. Beyond this, he denied any other medical problems and was not taking medications. The patient did exhibit a moderately high lipline.

Intraoral examination (Figure 2) revealed the absence of tooth #’s 1, 4, 5, 7, 10, 12, 16, 17, 20, 28, 29 and 32. Clinical evidence of possible horizontal alveolar ridge deficiencies was detected in site #’s 5, 7, 10, 12, 20, 28 and 29. Tooth #13 was over-erupted necessitating reduction of the buccal cusp to create space for an implant-supported crown.
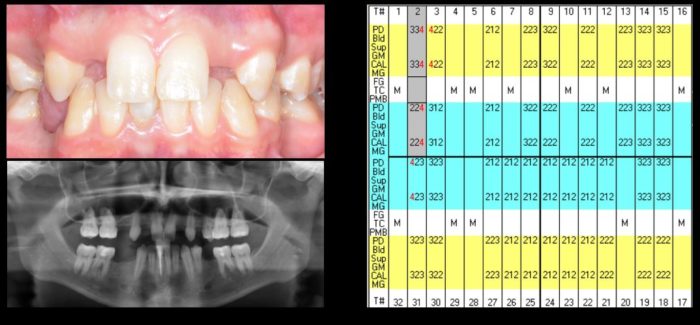
The patient exhibited mild gingivitis in the absence of any other periodontal pathology (periodontal charting in Figure 3). Both the maxillary and mandibular arches were U-shaped (Figure 4).

Radiographic evaluation (Figure 3) demonstrated a radiolucency at the apex of #25 and insufficient ridge height for implant placement in site #4. The lack of crestal bone height at this site was confirmed via a cone-beam CT scan that also showed a deficiency in ridge width in site #s 7 and 10.
Our Treatment Plan
With this diagnostic information, a treatment plan was presented to the patient that included endodontic therapy on #25, the placement of implants in site #’s 4, 7, 10, 12, 20, 28 and 29 that would all be restored as single-unit crowns and ceramic veneers on #’s 6, 8, 9 and 11.
It was explained to the patient that a lateral window sinus elevation was necessary for implant placement in site #4 and horizontal ridge augmentation in site #’s 7 and 10. The patient accepted the proposed plan and after an adult prophylaxis, the treatment was initiated.
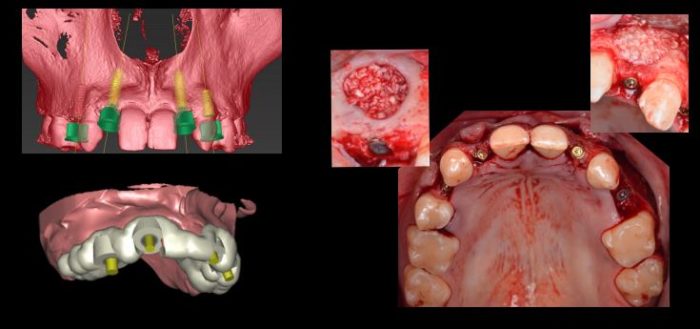
It was decided that the implants would be placed utilizing a computer-generated tooth-supported guide designed using Simplant (Figure 5) and that the sinus lift and horizontal ridge augmentations would be done coincident with implant placement. On the day of surgery (Figure 5), flaps were elevated and a lateral window sinus lift in site #4 was performed and grafted with BioOss that had been hydrated with recombinant platelet-derived growth factor (GEM-21).
Straumann Implants
Straumann bone level implants were then inserted as follows: site #’s 4 (4.1 x 10.0 mm), 7 (3.3 x 10.0 mm), 10 (3.3 x 10.0 mm), 12 (3.3 x 8.0 mm), 20 (3.3 x 8.0 mm), 28 (3.3 x 8.0 mm) and 29 (3.3 x 10.0 mm). Coverscrews were placed on all of the implants.

The same graft materials used in the sinus were utilized to augment the deficient ridge in site #’s 7 and 10. All of the grafts were covered with BioGide membranes. Goretex sutures were used to achieve tension-free primary closure of all of the flaps. After four months of uneventful healing, the implants were exposed and healing abutments were placed (Figure 6).
The maxillary implants were exposed using a carbon dioxide laser while the mandibular fixtures were uncovered via elevation of flaps. Two months after implant placement, the implant in site #4 was found to be mobile and was removed. The residual osteotomy was grafted with freeze-dried bone allograft and allowed to heal for three months at which time a Straumann bone level 4.1 x 10.0 mm implant was placed as a one-stage procedure.
The Restorative Phase

After four months of healing, all of the implants had successfully integrated and the restorative phase of therapy was begun. Impressions were made of the implants and custom abutments were fabricated (Figure 7). Tooth #’s 6, 8, 9 and 11 were prepared for ceramic veneers, an impression made and the teeth provisionalized.

Temporary crowns were placed on the implants. The patient was pleased with esthetics of the temporary restorations so the laboratory was asked to fabricate the final crowns and veneers that were then cemented in place (Figure 8).

Figure 9 shows a comparison of the patient’s pre- and post-treatment photographs, post-treatment radiographs and extraoral photograph. All of the implants appeared well-integrated and there was no evidence of periimplant soft tissue pathology. The patient was extremely satisfied with the function and esthetics of the final restorations.
The patient was treated in the post-graduate periodontics and periodontal prosthesis Amsterdam-Cohen Clinic of the University of Pennsylvania School of Dental Medicine. The treatment was carried out by Drs. Vico Cambra and Vu Dang La under the supervision of Drs. Howard Fraiman and Jonathan Korostoff.
(Dr. Jonathan Korostoff wrote this case study for other oral health care providers for our Dental Treatment Center Newsletter. He is the Professor of Periodontics and the
Director, Master of Science in Oral Biology Program at Penn Dental Medicine. He is the lead of the NFED Dental Treatment Center at Penn Dental Medicine. Read more of why Dr. Korostoff likes treating individuals affected by ectodermal dysplasias.)

